Olympus Corporation has issued a voluntary global labeling update for several of its bronchoscopic devices following serious safety concerns, including reports of endobronchial combustion events during procedures involving laser therapy, argon plasma coagulation (APC), or high-frequency cauterization. The update, released on October 31 and published by the FDA on November 3, 2025, is intended to reduce the risk of adverse events — one of which resulted in patient death — and ensure safer clinical use of its bronchofiberscopes and bronchovideoscopes.
What Happened?
Olympus announced that certain models of its bronchoscopes — specifically used in advanced pulmonary procedures involving energy-based modalities — required a labeling correction to better guide users on the risks of endobronchial combustion. The update covers both older bronchofiberscope models and newer bronchovideoscopes, which are commonly used in thoracic and interventional pulmonology.
The FDA’s safety communication outlines that Olympus is not recalling the devices, but is issuing a corrective action to improve labeling, user training, and clinical application guidelines. According to Olympus and the FDA, the updated labeling now includes more explicit warnings and usage limitations for procedures that involve oxygen-rich environments and high-energy tools, such as laser ablation, APC, or electrosurgical devices, which have been linked to combustion incidents inside the bronchial tree.
At least one adverse event resulting in patient death was included in the FDA’s analysis, prompting Olympus to proactively distribute revised labeling and notify affected facilities worldwide.
This labeling correction is not a simple technical note — it carries significant implications for multiple stakeholders across the surgical and procedural ecosystem:
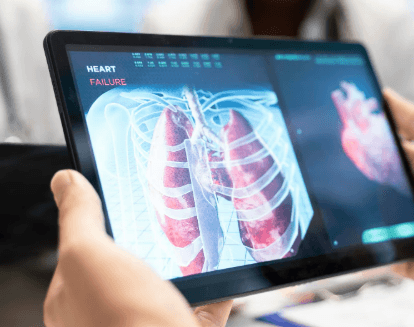
• Increased Clinical Risk Awareness: Bronchoscopes are used in many hospital systems for diagnostic and therapeutic interventions in the airways. Procedures involving oxygen administration and heat-producing instruments (like lasers or APC) carry combustion risks that can have fatal consequences. The updated labeling provides clearer clinical parameters to reduce those risks.
• Operational Disruption and Compliance: OR managers, endoscopy units, and pulmonary labs must review their Olympus devices to determine whether updated labels are required. Hospital compliance departments will also need to ensure that staff are re-trained on the new guidance to maintain Joint Commission and CMS compliance.
• Procurement and Device Management: Biomedical engineering and purchasing departments must document the update, ensure inventory records reflect the affected models, and confirm that updated materials are implemented in all clinical settings. Hospitals may also consider whether backup scopes or alternate vendors are needed if procedures must be paused or equipment rotated for safety checks.
• Vendor Communications and Liability Risk: Distributors and Olympus representatives must coordinate to ensure that all affected clients receive proper notification and revised documentation. Failure to do so could increase litigation or liability risk in case of additional adverse events.
Hospital and ASC administrators managing thoracic, pulmonary, and general surgery services using Olympus bronchoscopic systems.
Clinical teams, including interventional pulmonologists, thoracic surgeons, anesthesiologists, and respiratory therapists who routinely operate energy-based tools through bronchoscopes.
rocurement officers and biomedical engineers responsible for tracking medical device updates, labeling changes, and ensuring safe usage of instrumentation across multiple departments.
Distributors and Olympus field service reps tasked with executing the global corrective action and maintaining client support.